What causes the disease
The subcutaneous mite lives on the human head almost constantly, but does not cause aggravation in healthy people. Severe symptoms occur with a sharp decrease in immunity when the parasite affects the deep layers of the skin. Also, the activation of the Demodex mite depends on the functioning of the sebaceous glands of the head, the endocrine system and the general resistance of the body.
Factors contributing to the proliferation of hair mites in humans:
- hormonal disorders;
- long-term use of antibiotics and corticosteroids;
- chemical effects on the scalp;
- incorrectly selected hair care products;
- alcohol abuse and smoking;
- unbalanced diet with a predominance of salty, smoked, spicy foods;
- lack of vitamins;
- psycho-emotional overload;
- menopause or reaction to taking hormonal contraceptives.
It has been established that the Demodex parasite on the head secretes a special enzyme that affects the composition of human sebum and causes swelling of the skin. With strong immunity, inflammation and swelling go away on their own. But when the parasites are activated, their number increases to thirty pieces in one sebaceous gland. This contributes to the manifestation of symptoms of the disease on the skin.
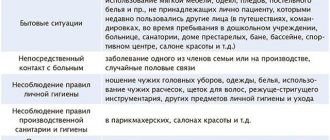
Demodex mites can be transmitted to others through direct contact, but the patient does not need to be isolated. In order for the disease to be transmitted to another, a number of factors must coincide, creating favorable conditions for the activation of the parasite.
Symptoms
Symptoms of the presence of a mite in the hair begin with the appearance of rosacea. This is pronounced erythema, occurring against the background of swelling and redness on the head, accompanied by acne nodules and ulcers on the skin.
Characteristic symptoms of demodicosis of the scalp:
- redness of the skin that may spread to the chest and upper back;
- papules (nodules), pimples and blisters filled with pus;
- thickening of the skin in the affected area;
- pronounced vascular network;
- dry skin, tightness, flaking and itching.
Such signs of the presence of a subcutaneous mite may initially be invisible. But as the Demodex parasite actively multiplies, a person feels severe discomfort. He develops dandruff, hair follicles are damaged, pimples appear not only on the forehead, but throughout the entire hair growth area.
Classification of demodicosis
ICD-10 code: B88.0.
For practical purposes, the clinical classification of demodicosis according to forms is used:
- Erythematous form: the leading symptom is redness and swelling of the skin;
- Pustular form: resembles acne vulgaris, occurs with the formation of acne on the skin, pustules ranging in size from 0.5 to 2 mm with pronounced perifollicular inflammation;
- Mixed form.
Damage to the eyes and eyelids deserves special mention. The parasite is able to inhabit the meibomian glands - modified sebaceous glands, the mouths of which open at the edges of the eyelids.
Demodicosis of the scalp occurs when parasites spread to the scalp.
Features of demodicosis in children
Children very rarely become infected with demodicosis, even with increased oily skin. Most often in childhood, the disease occurs in the form of blepharoconjunctivitis (inflammation of the eyelids and conjunctiva of the eye), resistant to treatment with antibiotics.
Which doctor treats demodicosis of the head?
First of all, you need to visit a dermatologist, who will give you a referral for tests and, based on their results, select a treatment regimen. For large areas of damage not only in the hair, but on the face, neck and back, the help of a dermatocosmetologist may be required. This is the doctor who determines your skin type. He will be able to select medicinal and cosmetic products and use them to treat problem areas. If the cause of the disease is poor immunity, the patient is referred to an immunologist. If hormonal disorders are suspected, an endocrinologist joins the treatment.
What is demodicosis: symptoms, diagnosis and treatment
Is your skin flaking and red, rashes appearing, or is itching bothering you? We go to a dermatologist for a diagnosis. With Vladislav Leonidovich Sheinkman, Candidate of Medical Sciences, dermatovenerologist at the Expert Tula Clinic, we are learning how to protect ourselves from demodicosis.
— Vladislav Leonidovich, what is demodicosis and what are the symptoms of this disease?
Demodectic mange is an infection of smooth skin and hair by microscopic mites of the genus Demodex. The mite lives in the sebaceous glands and hair follicles.
To date, 65 varieties of Demodex mites are known, 3 of which are relevant to humans, and the rest parasitize animals.
The mite is most often found on the skin of the face: nose, forehead, chin, as well as the eyelashes and eyebrows.
Clinical signs of demodicosis include redness of the skin, the appearance of nodules and pustules on it, itching, and increased secretion of sebum. If eyelashes or eyebrows are affected, the eyelids may become inflamed. A secondary bacterial infection and scar formation on the skin may occur.
— Is demodicosis the same as rosacea (rosacea) or are they different diagnoses?
Several decades ago, the mite Demodex folliculorum was believed to be the cause of rosacea.
It is currently known that this mite occurs in 90% of people, even with completely healthy skin. Therefore, according to modern ideas, it is believed that the mite can aggravate the course of rosacea.
If I detect signs of rosacea in a patient, that is the diagnosis I make. Even if a subsequent laboratory analysis reveals a mite, I will not make a diagnosis of demodicosis: according to the latest scientific data, its use is not entirely justified. Therefore, it makes no sense to look for differences between demodicosis and rosacea as two different diagnoses.
Sometimes it seems that many people have a kind of “demodecophobia.” The importance of this microorganism should not be exaggerated, if only because it is found in most people and often does not cause any symptoms.
— Demodicosis occurs only on the face or can it affect other parts of the body?
Classic localization is the face. Theoretically, a tick can be detected on the body, but in practice such a diagnosis makes no sense.
— For what reasons does demodicosis occur? Is this an infectious disease?
As I said earlier, Demodex folliculorum is present in most people and is an opportunistic mite.
Demodicosis is reflected in the section of infectious and parasitic diseases of ICD-10, but its classification as an infectious disease due to the conditional pathogenicity of the pathogen is debatable.
Under certain conditions (in particular, when the immune system is weakened - for example, under stress; overheating), Demodex multiplies, causing the clinical manifestations listed above.
An allergist-immunologist at Clinic Expert Smolensk talks about the signs of decreased immunity.
Chemova Ulyana Vladimirovna
— How is demodex mite transmitted?
By contact.
— Not only people, but also animals suffer from demodicosis. Can a person become infected with demodicosis from cats and dogs?
I believe not, since these mites are species specific.
— Why is demodicosis dangerous for humans?
There is no danger as such either for the person himself or for others. The main problem is cosmetic. This, in turn, adversely affects a person’s self-esteem and psychological state.
— Which doctor should you contact if you suspect demodicosis?
See a dermatologist. If eye symptoms are noted, consult an ophthalmologist according to indications.
You can make an appointment with a dermatologist here
Please note: consultations are not available in all cities
— Vladislav Leonidovich, how is demodicosis diagnosed? What tests should be taken if you suspect this disease?
First of all, a microscopic examination of skin flakes from the lesion. Since the manifestations of demodicosis develop against the background of some general disadvantage, according to indications, a consultation with related specialists (gastroenterologist, endocrinologist, neurologist) may be prescribed with appropriate additional research methods (general blood test and testing for hormones, ultrasound of the abdominal organs, etc. .).
Why is an abdominal ultrasound prescribed? The ultrasound diagnostics doctor at the Expert Orenburg Clinic, Anna Viktorovna Poskrebysheva, tells
— How is demodicosis treated?
First of all, strictly follow the doctor’s recommendations. Overheating in any form should be avoided (bath, sauna, bath, working in the sun, in the kitchen without an exhaust hood), as well as hypothermia; limit the use of cosmetics; do not eat hot food.
Sometimes patients, self-medicating, prescribe ointments with hormones. This should absolutely not be done, as it can lead to aggravation of the process.
Medications that affect ticks are prescribed. If there are pustules, use drugs with an antibacterial effect. Cryomassage is used - rubbing with pieces of ice prepared from tea, chamomile or string infusion. Cool herbal lotions and “talkers” based on sulfur, camphor alcohol and boric acid are also used. Treatment of demodicosis can be lengthy.
— What is the prognosis for demodicosis?
It depends on following the doctor's recommendations.
— Is it possible to cure demodicosis using medicines for animals?
It is unacceptable. Medicines for animals have their own specifics, so it is impossible to predict how they will affect humans.
— It is known that the success of treatment always depends not only on the doctor, but also on the patient himself. What does a patient need to do in order to defeat demodicosis once and for all?
Strictly adhere to the treatment regimen developed by a dermatologist, and under no circumstances self-medicate. Eat a healthy and balanced diet, eliminate harmful factors that aggravate the course of demodicosis. Limit, or better yet completely eliminate, the consumption of alcohol, hot, spicy, sweet foods, and coffee.
You might be interested in:
Herpes: how to recognize and cure?
At an appointment with a nutritionist. Soup: is it good or bad?
Themis will not give offense. Who protects the rights of patients in private clinics?
For reference:
Sheinkman Vladislav Leonidovich
Graduate of the pediatric faculty of the Smolensk State Medical Institute in 1994.
From 1994 to 1995, he completed an internship, and from 1996 to 1998, a clinical residency in the specialty “Dermatovenereology”.
Has an academic degree of Candidate of Medical Sciences.
Currently working at Clinic Expert Tula LLC as a dermatovenerologist. Provides reception at the address: st. Boldina, 74
Diagnostics
Treatment of demodicosis of the scalp begins with proper diagnosis. Even in a healthy person, the Demodex mite lives in the epithelial tissues, so doctors pay attention not to its presence, but to its quantity. The choice of the appropriate examination technique is made by the doctor, since each of the procedures has advantages and disadvantages.
Existing methods for diagnosing demodicosis:
- Scraping from the surface of the affected skin - with its help, the affected area of the skin is assessed and the parasite is calculated per unit of skin area.
- Examination of the secretion of the sebaceous glands - part of the mite elements is squeezed out, the skin on the head is partially damaged.
- Superficial biopsy - examines parts of the epithelium and the contents of its glands.
- Skin biopsy followed by histological examination allows you to examine the secretion of the sebaceous glands.
- The study of eyelashes and hair reveals parasites in the follicles; the procedure does not cause much pain.
Treatment
After receiving the test results, the doctor decides how to treat the disease, and the patient must complete the full course to avoid relapse. Therapy includes several areas - medications, skin care products and dietary nutrition.
Many patients prefer to use folk remedies. Doctors approve of this approach, because herbs and home recipes are safe, speed up recovery and complement the therapeutic effects of medications.
Immunity restoration
How to get rid of subcutaneous mites to prevent relapse of the disease? Since the parasite is activated when immunity decreases, it is necessary to restore the body's resistance.
List of drugs to strengthen immune defense and prevent demodicosis:
- vitamin complexes with a high content of phosphorus, calcium, iron and zinc;
- B vitamins and nicotinic acid;
- folic acid;
- Brewer's yeast;
- immunostimulating drugs in tablets and injections - Interferon, Cycloferon, echinacea tincture, Immunal.
If hair mites in people are activated under severe stress and emotional overload, they should be avoided. The doctor may prescribe sedatives.
In case of chronic demodicosis, drastic measures are taken to restore immunity - autohemotherapy. This is the introduction under the skin or intramuscularly to the patient of his own blood obtained from a vein.
Drug treatment
The use of medications for demodicosis is aimed at eliminating the mite and the consequences of its vital activity in the epithelial tissues. Metronidazole is used to treat the parasite. The first course lasts 6 weeks, during which the patient drinks 250 mg of the drug twice a day. After 2-3 weeks, the course is repeated, the dose of the medicine is the same.
In between, doctors prescribe 500 mg of purified sulfur taken orally along with meals twice a day. A five-day course is recommended to take Tinidazole 4 tablets per day and Hingamin 250 mg 2 times a day.
If the inflamed skin becomes covered with ulcers, and the patient scratches his head, causing a bacterial infection, antibiotics and antifungal agents are prescribed. These include Tetracycline, Erythromycin, Nystatin.
Folk remedies
In combination with strengthening the immune system and drug treatment of the skin, you can use traditional medicine recipes. These include washes, masks and scalp treatments.
Popular home remedies for hair mites:
- Tar soap - washing your hair inhibits the proliferation of parasites, cleanses the skin and restores its structure.
- Chatterbox - the product contains 10 tablets of Nystatin, Metronidazole and Levomycetin, ground into powder, as well as 100 ml of Dimexide and purified water. Prepare a fresh solution and treat the affected areas of the head with it for 2 weeks, 2 times a day.
- Calendula and Demalon ointment - in the morning you need to rinse your hair with water, after 15 minutes apply calendula tincture, and after 5 minutes spread the ointment on your skin. Leave the mask on until the evening, then wash your hair and treat with the tincture. The course of treatment is 30 days.
How to treat demodicosis with purified kerosene depends on how severely irritated and inflamed the scalp is. The product is applied to the affected areas for three days, then washed off. Kerosene cuts off the parasite's nutrition and access to oxygen due to the film created on the skin, which causes the tick to die.
If you do not want to prepare products according to folk recipes, you can purchase ready-made pharmacy shampoo that cures demodicosis. It can be used daily or as recommended by your doctor.
Shampoos
Treatment of demodicosis with shampoos helps to treat hard-to-reach areas of the skin. The products allow you to eliminate the symptoms of the disease on the skin, destroy mites and restore damaged epithelium after damage.
The most effective shampoos against hair parasites:
- Demodex Complex – reduces the number of mites, cleanses the skin of scales and dead particles. Used in treatment and prevention.
- Stop Demodex – relieves irritation, soothes the epidermis, suppresses the proliferation of parasites. For the best effect, apply the product to the head several times and leave for 3-5 minutes.
- Demodex Ovante is a natural-based product from an American manufacturer. Contains oils, vitamins, zinc, sulfur and plant extracts. Does not cause an allergic reaction, suitable for daily use for 14-28 days in a row.
Shampoos for the treatment of demodicosis are used simultaneously with medications and other external agents for better effect.
Diet
To achieve lasting results, in addition to cosmetics and medications, doctors recommend following a special diet. It is built according to the type of treatment table No. 5. The patient must adhere to proper nutrition during the entire course of therapy, in which case demodicosis of the scalp goes away faster.
It is necessary to exclude alcohol, spicy, salty and smoked foods, and sweets. To prevent blood from rushing to the head and the proliferation of parasites, food and drinks should be warm.
You cannot overeat; all food should be light, but nutritious. Preference is given to fruits, grains, vegetables, fiber, and herbs. It is recommended to consume low-fat meat and fish. Dairy and fermented milk products are beneficial.
Rules for caring for the scalp and hair during treatment
In the process of treating demodicosis of the skin, certain rules should be followed. Shampoo alone will not cope with the attack of parasites. Therefore, it is necessary to wash your hair with a medicinal product, and then reinforce the result with folk methods. Due to the fact that mites are most active in the evening and at night, it is best to treat the skin during this period.
Products in the form of scrubs are not recommended for use more than once every 7 days, so as not to disturb the natural oil balance of the skin and not damage it. Infusions of eucalyptus, oak bark, buckthorn, elecampane, and wormwood have a beneficial effect on the scalp and hair. Your hair should be washed daily. During treatment, hair coloring and perming should not be done.
Symptoms of demodicosis
Facial skin
Most often, demodex lives on the skin of the face, affecting the forehead, cheeks and chin, nasolabial folds, skin around the lips, and the area of the brow ridges. Moreover, the tick does not sit still, but slowly moves under the skin (especially active in the evening and at night), which causes itching and a feeling of “goosebumps” under the skin.
Among the external manifestations, the symptoms of demodicosis are redness, inflammation, peeling, rosacea, and pimples. The latter may be signs of problems associated with demodicosis - rosacea or acne.
Ophthalmodemodecosis
The eight-legged mite can even affect the eye area - here it lives in the hair follicles at the roots of the eyelashes. As a result, a specific eye lesion develops – demodectic blepharitis. Symptoms include itching and swelling, plaque along the edges of the eyelids, and the appearance of scales at the base of the eyelashes. In addition, demodex can provoke eyelash loss, frequent stye, blepharoconjunctivitis and other troubles.
Demodicosis of the scalp
Demodex is quite comfortable on the scalp - it is also easy to profit from sebum there. And then “reward” the person with dandruff, irritation, itching or hair loss. At the same time, few people think that the culprit of such troubles may be a subcutaneous mite, and not a poorly selected shampoo, low-quality hair dye, etc.
Prevention
To avoid infection with demodicosis, you should not use other people's bed linen and hygiene items. Linen should be changed frequently and ironed thoroughly. Feather pillows may contain mites, so it is worth replacing them with ones made of synthetic materials.
If itching and flaking appear, especially if you previously had demodicosis, do not comb or scratch the skin. It is better to immediately consult a doctor to be examined for ticks.
You should stop smoking and drinking alcohol, especially during treatment for parasites. Immunity needs to be increased by hardening, walking in the fresh air, playing sports and taking multivitamin complexes.
Demodicosis of the scalp is a disease that is provoked by several reasons. If a person has problems with the immune or endocrine system, or increased sebum production, then treatment will be aimed at eliminating these pathologies. Following medical recommendations, a combination of medications and folk remedies, as well as regular prevention will lead to quick positive results and lasting remission.
Author: Marina Ermakova, doctor, especially for Dermatologiya.pro
The first signs of demodicosis:
- The appearance of various rashes on the skin: pimples, pustules, ulcers, blackheads, etc. All of them can indirectly indicate the rapid proliferation of mites in the skin. If demodicosis is not treated, acne begins to form on the back, chest and thighs;
- The skin becomes covered with red and dense spots, sometimes they are confused with manifestations of rosacea;
- Increased activity of the sebaceous glands. In areas of demodicosis, the skin becomes shiny and greasy, this is especially true for the nose and cheeks;
- Due to multiple rashes and red spots, the skin takes on a bumpy appearance. The formation of connective tissue increases;
- The skin is very itchy and there is a periodic crawling sensation. The itching intensifies at night, but often patients do not pay attention to it and do not rush to see a doctor. And when scratching, microtraumas form on the skin, which only increases the severity of the symptoms of the disease;
- Hair loss and burning sensation, causing scratching of the scalp. Early baldness may be one of the symptoms of demodicosis in humans;
- Itching and loss of eyelashes and eyebrows. The hair becomes thinner, and the burning sensation only contributes to the loss due to constant scratching.
- Unbearable desire to scratch in the area of the ears.
When you try to wash your skin with soap, the symptoms begin to worsen: red spots appear, itching and burning intensify. The condition of the skin becomes more deplorable when tanning in the sun or in a solarium, while in the pool, or when using fatty creams.